Hands Only CPR Helps Save Lives
April 10th, 2019 A Swedish review of out-of-hospital cardiac arrest data shows that rates of bystander CPR nearly doubled; compression only CPR increased six-fold over a 18 year period; and the chance of survival was doubled for any form of CPR compared with no CPR, according to new research in the American Heart Association’s journal “Circulation.”
A Swedish review of out-of-hospital cardiac arrest data shows that rates of bystander CPR nearly doubled; compression only CPR increased six-fold over a 18 year period; and the chance of survival was doubled for any form of CPR compared with no CPR, according to new research in the American Heart Association’s journal “Circulation.”
Compression Only CPR
Due to the emergence of compression only CPR as an alternative to standard CPR (chest compressions and mouth-to-mouth rescue breaths) researchers analyzed the impact of the simpler, hands only CPR technique and the association between the type of CPR performed and the patient survival for 30 days.
Findings come from research conducted between 2000 and 2017. The study included more than 30,000 participants and showed that nearly 40 percent received CPR from a bystander that included mouth- to-mouth and 20 percent received hand compressions.
The American Heart Association says immediate CPR can double or triple chances of survival after cardiac arrest. Keeping the blood flow active, even partially, extends the opportunity for successful resuscitation once trained medical staff arrive on site.
Cardiac Arrest
Cardiac arrest is the abrupt loss of heart function. It can come on suddenly and often is fatal if appropriate steps aren’t taken immediately. Before giving a person CPR:
- Check the scene around the person: Check to make sure the scene is safe, tap the person on the shoulder to see if they’re ok, and look for signs of rhythmic, normal breathing.
- Call 911 for assistance: If there’s no response from the victim when asked if he or she is ok, call 911 or ask a bystander for help.
- Begin compressions if the person is unresponsive: Perform hands only CPR.
According to the American Red Cross the steps to performing hands only CPR are:
- Kneel besides the person who needs help.
- Place the heel of one hand on the center of the chest.
- Place the heel of the other hand on top of the first hand, and then lace your fingers together.
- Position your body so that your shoulders are directly over your hands, and keep your arms straight.
- Use your body weight to help you administer compressions that are at least two inches deep and delivered at a rate of at least 100 compressions per minute. Just be sure to let the chest rise completely between compressions.
- Continue hands only CPR until: you see obvious signs of life, like breathing, another trained responder or emergency medical professional can take over, or you’re too exhausted to continue, an AED becomes available, or the scene becomes unsafe.
What IAA has to Say
Insurance Administrator of America hopes everyone can take the time to learn how to administer CPR from a certified professional. IAA wants you to remember that you never know when it will help save a life!
Like this blog post? Let IAA know by going to our Facebook page and clicking the Like button!
FDA Approves First Drug to Treat Postpartum Depression
April 3rd, 2019
New Drug Treatment
The drug, announced on March 19, will be known as Zulresso and is given in an IV over a three day period in a hospital setting.
Zulresso rebalances hormones that spike during pregnancy and plummet after birth. Unlike conventional anti-depressants, the effect can be almost immediate. Zulresso has a synthetic form of the hormone allopregnanolone in it. The hormone increases throughout a woman’s pregnancy and then plummets after she gives birth, a possible contributor to postpartum depression.
In double-blind placebo controlled trials, many women with moderate to severe postpartum depression saw a marked improvement of their symptoms within just 24 hours of receiving the drug. The improvement was still present 30 days after the infusion, the length of the trial. Common side effects were drowsiness and dizziness. The drug is not believed to have any long-term safety concerns.
The trials were conducted in 2016 and 2017, and involved more than 200 women who had symptoms of postpartum depression.
The drug should be available by June.
Up until now, new mothers experiencing postpartum depression have been prescribed the same anti-depressants used for treating depression in the general population. They do not address the hormonal changes that women go through during and after a pregnancy.
Researchers stress that women need to be screened and discuss all treatment options with their physician.
Postpartum Awareness
In the United States, about one in nine mothers experience depression after having a baby.
According to the Centers for Disease Control and Prevention (CDC), postpartum depression is “intense sadness, anxiety or despair that occurs within the first year after giving birth.” Signs and symptoms include:
- Depressed mood or severe mood swings
- Difficulty bonding with the baby
- Diminished ability to think clearly, concentrate or make decisions
- Excessive crying
- Fear that you’re not a good mother
- Feelings of unworthiness, shame, guilt, or inadequacy
- Hopelessness
- Insomnia or sleeping too much
- Intense irritability and anger
- Loss of appetite or eating much more than usual
- Overwhelming fatigue or loss of energy
- Reduced interest and pleasure in activities you use to enjoy
- Restlessness
- Severe anxiety or panic attacks
- Thoughts of harming yourself or your baby
- Withdrawing from family and friends
Postpartum depression afflicts as many as 400,000 women in the United States each year.
What IAA has to Say
Insurance Administrator of America wants to keep you up to date on the world of health. Remember, with IAA one call does it all.
Like this blog post? Let IAA know by going to our Facebook page and clicking the Like button!
Aspirin may not be the Answer to Heart Attack Prevention
March 27th, 2019 According to new guidelines published on March 18 by the American College of Cardiology, not enough evidence exists to show that aspirin can help prevent heart attacks and strokes.
According to new guidelines published on March 18 by the American College of Cardiology, not enough evidence exists to show that aspirin can help prevent heart attacks and strokes.
New Guidelines
Have you been relying on aspirin to prevent a heart attack or stroke? That may no longer be the best prevention method. New recommendations say that a person’s risk of life-threatening bleeding should be factored into their decision whether or not to start taking aspirin to prevent heart attack or stroke.
Aspirin is made of salicylic acid. It works by stopping cox-1, a specialized protein in our body that activates a type of cell called a platelet. These are found in our blood and are responsible for making it sticky. When platelets pile up, a clot can form. If the clot forms in the heart, a heart attack can occur; if the clot forms in the brain, a stroke is possible. By interfering with platelet function, aspirin can potentially prevent a heart attack or stroke, but the blood can also become less sticky and a person can become prone to bleeding in general.
A large study in 2009 and three studies in 2018, showed that the rate of significant bleeding related to aspirin were similar or even greater than the rate at which it reduced a first time heart attack or stroke.
Instead, people should use statins and make lifestyle changes to prevent cardiovascular risk. For people between the ages of 40 and 70 who are at high cardiovascular risk, but low bleeding risk, new guidelines recommend low-dose aspirin every day.
Decades of data support the use of aspirin for the secondary prevention of cardiovascular disease, meaning a repeat heart attack or stroke.
Preventing Cardiovascular Disease
When it comes to cardiovascular disease, prevention is key!
- Ban smoking
- Be smart about cholesterol: When blood flows through your blood vessels, it can drop traces of cholesterol, fat and calcium, creating a buildup of plaque in your arteries. Too much of that plaque makes a heart attack more likely.
- Check your weight: If you have extra pounds, it can put your heart at risk. Exercise and a good diet help.
- Keep tabs on your blood pressure: If it’s too high, your risk of a heart attack and heart disease goes up.
- Mind your blood sugar: Too much sugar in your blood can damage your arteries.
- Take it easy: Find a relaxation method that works for you. Stressful emotions such as anger and hostility may lead to heart attack risk, so keep calm and be cool.
It is also a good idea to be social. Research shows that people with more social support are less prone to heart trouble.
What IAA has to Say
Insurance Administrator of America wants to keep you up to date on the world of health. Remember, with IAA one call does it all.
LIke this blog post? Let IAA know by going to our Facebook page and clicking the Like button!
New Guidelines Issued for Food Allergy Prevention
March 20th, 2019 On March 18, the American Academy of Pediatrics (AAP) published updated guidance on the prevention of food allergies and other allergic conditions.
On March 18, the American Academy of Pediatrics (AAP) published updated guidance on the prevention of food allergies and other allergic conditions.
New Guidelines
The new guidelines were based on a detailed review of all available evidence on the topic. According to the report, there is no convincing evidence that delaying the introduction of allergenic foods beyond four to six months of age, works in preventing food allergies. In addition, there is strong evidence that purposeful, early introduction of peanuts as early as four months may prevent the development of a peanut allergy in infants at high risk.
No evidence was found that avoiding allergenic foods during pregnancy or breast feeding, worked in the prevention of allergenic conditions. Neither did the use of hydrolyzed formulas, even in kids who were at high risk.
This study, known as the Learning Early About Peanut (LEAP) trial, showed that children at high risk of developing peanut allergies who are introduced to peanuts at four to six months old, had a significantly lower risk of developing a peanut allergy than those who waited until they were five years old.
Thoughts on this issue have certainly changed over time; in 2000, the AAP recommended delaying the introduction of peanuts until three years old.
Food Allergy Signs and Symptoms
Food allergies can cause serious and even deadly reactions. With a food allergy, the body reacts as though that particular food product is harmful. As a result, the body’s immune creates antibodies to fight the food allergen. Every time the person eats, or in some cases handles or breathes in the food, the body releases a chemical like histamine. This triggers an allergic reaction that can affect the respiratory system, gastrointestinal tract, skin, or cardiovascular system. Symptoms in children can include:
- Belly pain
- Coughing
- Diarrhea
- Hives
- Hoarseness
- Itchy, watery or swollen eyes
- Red spots
- Swelling
- Throat tightness
- Trouble breathing
- Vomiting
- Wheezing
The most common foods that cause allergies are:
- Milk
- Eggs
- Soy
- Wheat
- Tree nuts
- Peanuts
- Fish
- Shellfish
In general, most kids with food allergies outgrow them. It is estimated that 80 to 90 percent of egg, milk, wheat, and soy allergies go away by the age of five.
What IAA has to Say
Insurance Administrator of America knows that food allergies can be serious, so be sure to be on the lookout for any signs of a reaction when introducing your child to new foods. Remember, with IAA one call does it all.
Interested in reading more on this topic? Click here and here!
Health in the News: Luke Perry’s Death Sheds Light on Strokes
March 13th, 2019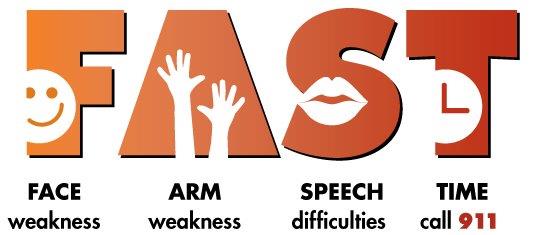 Luke Perry known for his roles on “Beverly Hills, 90210” and “Riverdale” died on March 4, after suffering a massive stroke days prior.
Luke Perry known for his roles on “Beverly Hills, 90210” and “Riverdale” died on March 4, after suffering a massive stroke days prior.
Stroke Signs and Symptoms
Each year more than 795,000 Americans suffer from a stroke, according to the Centers for Disease Control and Prevention (CDC).
Signs of a stroke can include:
- Sudden confusion, trouble speaking or difficulty understanding speech
- Sudden numbness or weakness in the face, arm or leg, especially on one side of the body
- Sudden severe headache with no known cause
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance, or lack of coordination
If your symptoms go away after a few minutes you may have had a transient ischemic attack (TIA). Although brief, a TIA is a sign of a serious condition that will not go away without medical help.
F.A.S.T. Test
During a stroke, every minute counts. Fast treatment can lessen the brain damage that a stroke can cause. That’s why it is important to remember the F.A.S.T. Test:
- F-Face: Ask the person to smile. Does one side of the face droop?
- A-Arms: Ask the person to raise both arms. Does one arm drift downward?
- S-Speech: Ask the person to repeat a simple phrase. Is the speech slurred or strange?
- T-Time: If you see any of these signs, call 911 right away.
The stroke treatments that work best are available only if the stroke is recognized and diagnosed within three hours of the first symptoms.
Strokes are responsible for about one out of 20 deaths in the United States, making it the fifth leading cause of death among Americans.
What IAA has to Say
Insurance Administrator of America wants you to know the signs of a stroke and how to detect when a stroke is happening to someone. IAA knows that when it comes to strokes, timing is everything, so if you believe someone is having a stroke, take action right away.
Interested in reading more on this topic? Click here!
